“Don’t use virgin coconut oil! Or stearic acid! They’re so comedogenic!”
… are they, though?
And is “non-comedogenic” alone the one magic, major thing to prevent acne? The internet is a wonderful source of good information…but also outdated information, information without context, incomplete information, and wrong information. Comedogenicity, for example, has had a complex history with conflicting results and different testing methods. Yet many sites that list comedogenic ingredients don’t show the sources of the studies and how the studies have held up over time. And it seems that comedones are only half the story. To really help keep acne at bay, we need “hypoallergenic” and “anti-inflammatory” as much as “non-comedogenic.”
To help “unclog” some of the confusion, we asked dermatologist and dermatopathologist Dr. Vermén Verallo-Rowell to explain: what do “comedogenic” and “acnegenic” mean, and what studies should we be trusting?
What we learned…
See Dr. Verallo-Rowell’s original summary below. These are 3 of the most eye-opening things that we learned.
1. Non-comedogenic isn’t all that you need to prevent acne. Look for: non-comedogenic, no contact allergens, no irritants, and anti-inflammatory.
First, let’s clarify what’s what…
Comedones and comedogenic:
“Comedone” is the medical term for a plugged hair follicle. Hormones, other inflammatory stress triggers, as well cosmetics and skincare and/or their ingredients can form comedones. When they’re closed, they’re whiteheads. When they’re open, they’re blackheads. They might be visible or not (micro-comedone).
What clogs the follicle — the product itself and/or its ingredient(s) — is a comedogen(s).
Acne and acnegenic:
Acne is caused by inflammation. There can be many triggers, from an inflammatory diet, hormones, a medical condition, and certain drugs. A cosmetic product or its ingredients can also be a trigger — here, the product/ingredients may cause an irritant contact dermatitis that also becomes inflamed. Acne starts as a comedone (clogged hair follicle). Sebum production follows, then an overgrowth of a microbe in the follicle (innate bacteria, fungi, or mites), which leads to more inflammation and the formation of papules, pustules, and/or cysts.
What clogs the follicle but also causes irritation and possibly inflammation — the product itself and/or its ingredient(s) — is an acnegen(s).
What should I be looking for?
Comedogens (which clog the follicle) are not necessarily acnegens (which clog then irritate the follicle, and cause inflammation); and acnegens are not necessarily comedogens
A product that says “non-comedogenic” should have done tests on the ingredient and final product — and/or is relying on studies already done on the same ingredient — to prove that it does not clog pores. “Non-acnegenic” may be the better term to look for if you’re trying to prevent acne in addition to clogged pores but many FDAs prevent the use of this term for cosmetic products (both “acne” and “inflammation” are restricted to drugs). The best thing would be to look for products that:
• Say “non-comedogenic”;
• Have zero of the top contact allergens and irritants; and
• Are anti-inflammatory.
Remember that comedogens clog pores. Acnegens both clogs pores and cause irritation and inflammation. A non-comedogenic product with anti-inflammatories and without allergens or irritants should fit the bill. Just make sure that the brand relies on Human Controlled Use Tests or similar studies on people to determine comedogenicity and/or acnegenicity because…
2. Most of the studies used to determine “comedogenicity” are old and inconsistent or inaccurate.
Part of the confusion lies in that the most commonly cited studies for comedogenicity are old, done on rabbit ears (Rabbit Ear Assays; “REA”), and are less reliable. Just ten years after some of the earliest studies that were considered the gold standard for comedogenicity, the same team of doctors, using a human skin model in lieu of the Rabbit Ear Assay, saw that the results of their initial animal (and later human) studies were incongruent.
To try to resolve the difference, in 1989, the American Academy of Dermatology held the Symposium on Comedogenicity to standardize testing methods. To clarify findings, especially if positive in REAs, it was recommended that “the product should be adequately tested in humans before general use.” Results from tests on humans were considered the defining results.
The next wave of influential studies began in 2006 with Draelos et al. One study concluded that finished cosmetics with ingredients shown to be comedogenic in Rabbit Ear Assays are not necessarily comedogenic when tested on human skin. More recent studies use updated methodology that measure oil production and tackle inflammatory follicular targets. These seem to more accurately identity what ingredients or products are comedogenic and acnegenic.
Draelos’s results, the results from tests on human skin, as well as newer methodologies are what we use in our research center and when formulating VMV Hypoallergenics products.
The newer methodologies have many advantages: they are more accurate, they don’t need bunnies, they are easy to perform on more subjects for greater statistical significance, and they can be done with more types of ingredients, finished products, and other materials. Importantly, unlike REAs which were incongruent themselves and incongruent when compared to human tests, these newer methods are more consistent and are accurately reproducible. And, in case you were wondering, these show virgin coconut oil as not comedogenic. Virgin coconut oil is also not acnegenic.
3. What is causing your acne may not be what you think.
The easiest thing to blame is the last product you used or a new product you’re trying. But acne (especially adult acne) is multi-factorial: it can have many possible causes. Some causes include certain cosmetic products, and using too many cosmetic products, but also hormones, certain medical conditions, disinfectants, some medication, lack of sleep, halogens (fluoride, chloride, iodide, etc.), and inflammatory food (red meats and byproducts, highly processed foods, junk food, too much carbs and dairy, “white” food like white rice and bread, pre-packaged drinks, vegetable oils, etc.).
A product that produces a reaction quickly might be acnegenic: it clogs the pore but also causes irritation (remember, acne in this case is actually a type of irritant contact dermatitis of the follicle) and inflammation. On the other hand, a product that is comedogenic would take time (sometimes weeks) to show a reaction because more applications are needed for the erring ingredient/s to build up and cause clogging.
If you’re convinced that a product that you used is the problem because you noticed new acne soon after using it, maybe the product is acnegenic: it contains both comedogens but also allergens and irritants that have irritated the pore and caused inflammation. If the lesions developed over time, it might be due to the comedogens in your most recent product or in your other products that have had enough time to build up and clog your pores. Or it could be a change in lifestyle (more stress, lack of sleep, worse food), new medication, a development in hormones, or even a condition that just looks like acne but isn’t. This is why your best bet is to see a dermatologist for a comprehensive history, tests, and a proper diagnosis.
For guidance, a lot of people search online and stumble upon “comedogenicity tables” on acne websites. Most of the tables are adapted from the Kligman Rabbit Ear Assay studies and Fulton collation of these studies. As a review of medical literature shows that these are incongruent at best: what is consistent is the inconsistency of results between Rabbit Ear Assays and human skin studies.
This well established incongruence between REAs and human studies, along with the difficulty in reproducing the results of REAs, led to the official AAD Symposium Consensus Statement saying that human skin tests are the determining results. We therefore rely on human skin tests with newer methodologies (like Human Controlled Use Tests) and not on older Rabbit Ear Assays that have been proven wrong or proven to be difficult to reproduce with the same results.
Summary by Vermén M. Verallo-Rowell, MD, FPDS, FAAD, FASDP, FADA
The concept of acnegenic and comedogenic to describe ingredients individually, and in skin care and cosmetic products, has been based on animal and human test protocols. The results are varied and standards not well defined for manufacturers or by regulatory bodies. Hence the confusion for the users of these products and the meaning and use of these terms.
Acnegenic products induce comedones plus inflamed papules, pustules, and cysts. The cause of acnegenicity is follicular irritation. It is a variant of irritant contact dermatitis with a more pronounced follicular component. As such, acne lesions appear quite quickly after application, while comedones may take weeks to develop. Therefore, comedogenic substances are not necessarily acnegenic, and the reverse is also true.(1)
Comedogenicity is the potential of a cosmetic or of its components to form acne-like plugged hair follicles that, when closed, are called whiteheads and, when open, are called blackheads. The medical term for both is a comedone. Chloracne, a form of comedonal acne was first seen among factory workers through the 1940s. Using the Rabbit Ear Assay (REA), chloracne was shown to be due to chlorinated hydrocarbons.(2) Kligman in 1970 used the REA to rate the comedogenicity of human sebum on a scale of 0 (no potential) to 3 (severe potential).(3) In 1972 Kligman and Mills next linked REA comedogenicity ratings of human sebum and cosmetic ingredients to low-grade acne which they called “cosmetic acne” in the cheeks of 22-25 year old post-adolescent young women.(4)
Ten years later, Mills and Kligman continued to do comedogenicity studies on the same chemicals, but used a human skin model in lieu of the rabbit ear. Surprisingly, the results of their initial animal, and later human, studies were incongruent.(5)
To try to resolve the difference, the American Academy of Dermatology in 1989 held the Symposium on Comedogenicity to standardize testing methods. They came up with the following consensus statement: “If the animal model does not show evidence of comedogenesis, the test material under consideration is unlikely to be comedogenic in human skin. One plus (+) positive reactions are also unlikely to cause reactions in humans. Two (++) or three (+++) responses require sound scientific judgment. Reformulation should be considered, or the product should be adequately tested in humans before general use.”(6)
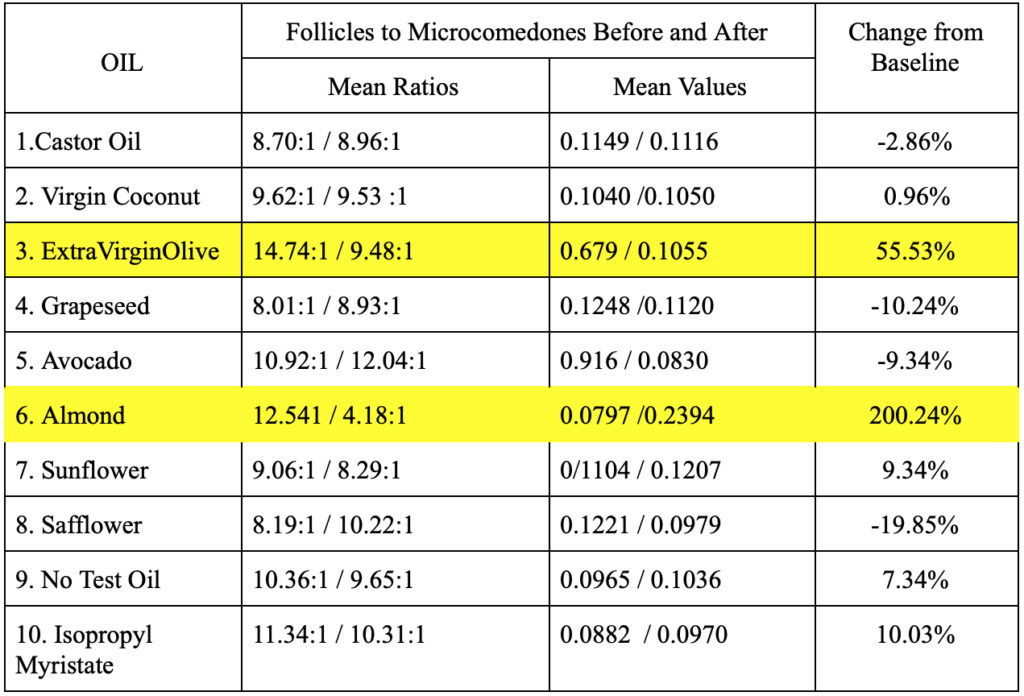
These findings lead to a study in 2006 by Draelos on six individuals with prominent follicular orifices and the ability to form comedones on the upper aspect of the back which served as the test sites. Using the technique of Marks and Dawber, 0.2 to 0.5 mL of 7 cosmetics with at least 2 ingredients reported to be comedogenic in the REA assays, a positive, and a negative control were applied, kept covered for 48 hours, opened, and re-applied 3 times weekly for 4 weeks. Cyanoacrylate follicular biopsies at baseline and at the end of the study counted the ratio of follicles to microcomedones per square inch. Like Kligman, Draelos’ results were likewise “incongruous”. The study concludes that finished cosmetics with ingredients shown to be comedogenic in rabbit ear testing, are not necessarily comedogenic when tested on human skin.(7)
In recent years, dermatologists have noted the rise of cases of adult acne defined as acne in men or women 25 years and older. Unlike adolescent acne which occurs from hormonal surges in adolescence(8), adult acne is multifactorial. The factors include hormones from stress-related fluctuating hormones of fast-paced modern lifestyles; polycystic ovarian syndrome; and discontinuing birth control pills. Commonly used drugs and chemicals such as antidepressants, cough medicines, corticosteroids including those in inhalers; pollutants like particulates, chlorines and dioxins in our environment, and in our food and drinks are others. Lastly, the increasing number of chemicals in cosmetics and cosmeceuticals are frequent suspect causes.(9,10) Quality of life among adolescents to adults with acne have been shown to be as serious as in those with diseases considered to be dire such as CVD, diabetes, and cancer.(11-13)
More recent studies are now used to characterize sebum production, and inflammatory follicular targets that may be useful to more accurately characterize what ingredients or products are indeed comedogenic and acnegenic.(14,15 )
A study by Catambay, Villanueva and Verallo-Rowell in 2016 modified the Draelos human comedogenicity assay (DHSA). The study again proved that although there were some similarities of REA and DHSA ratings in 3 oils, the 5 others had different readings. Similar were DHSA (and REA) – comedogenic Olive and Almond; DHSA (and REA) – non-comedogenic Castor. Dissimilar were DHSA non-comedogenic Coconut, Avocado and Grapeseed (REA comedogenic); DHSA non-comedogenic sunflower and safflower (REA mildly comedogenic) oils. Notable is coconut which, despite years of being listed as comedogenic (in REA ratings), was shown non-comedogenic by DHSA, Table 1. This confirms what has been seen in clinics where VCO, for regular application not just on the face, but also all over the body, is a non-comedogenic moisturizer and antiseptic oil. The study utilized a new methodology with many advantages: accurately reproducible, easy to perform, cost effective, can be done on a larger number of test materials (ingredients, finished products), on a bigger subject size for greater statistical significance of results, and “no animal testing” for cosmetic ingredients and cosmetic products.(17)
Consumers tend to immediately blame cosmetics for their adult acne and look for self-help guidance to the comedogenicity tables found in the internet (acne websites) or even in dermatology literature. Most of the tables are adapted from the Kligman (0-3) ratings and Fulton who collated the REA studies and rated comedogenicity and also irritancy as (0 to 5). All are based on REA assays.
References:
- Draelos ZD. Atlas of Cosmetic Dermatology. Philadelphia, Pennsylvania: Churchill Livingstone, 2000, pp. 25-29.
- Moses M, Lilis R, Crow KD, et al. (1984). Health status of workers with past exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin in the manufacture of 2,4,5-trichlorophenoxyacetic acid: comparison of findings with and without chloracne. Am. J. Ind. Med. 5 (3): 161–82. doi:10.1002/ajim.4700050303. PMID 6142642
- Kligman A.M., Wheatley V.R., Mills O.H. Comedogenicity of Human Sebum. Arch Dermatol 1970 Sep;102(3):267-75.PMID: 4247928
- Kligman AM, Mills OH. Acne cosmetica. Arch Dermatol. 1972;106:893-897
- Mills OH, Kligman AM. Human model for assessing comedogenic substances. Arch Dermatol. 1982;116:903-905.
- Consensus Statement, American Academy of Dermatology Invitational Symposium on Comedogenicity. J Am Acad Dermatol. 1989;20:272-277.
- Draelos ZD, DiNardo JC. A re-evaluation of the comedogenicity concept. J Am Acad Dermatol. 2006;54:507-512.
- Smithard A, Glazebrook C, Williams HC. Acne prevalence, knowledge about acne and psychological morbidity in mid-adolescence: a community-based study. Br J Dermatol. 2001;145:274-279.
- H. P. M. Gollnick H.,P.,M. Review: From new findings in acne pathogenesis to new approaches in treatment. 07 June 2015 https://doi.org/10.1111/jdv.13186
- Verallo-Rowell V.M. Chapter 7. Role of diet and environment in skin ageing. In:Ageing and Longevity Medical Webinars Handbook. Genuino RF, Genjuino LS, Arquiza MC, eds.Manila, Philippines: Mu Sigma PhiSoririty Inc. June 2020.
- Barnes, LE, Levender,MM, Fleischer Jr, AB, Feldman, S.R. Review Quality of Life Measures for Acne Patients. Dermatol Clin 2012 Apr;30(2):293-300, ix. doi: 10.1016/j.det.2011.11.001
- Mallon E, Newton JN, Klassen A, Stewart-Brown SL, Ryan TJ, Finlay AY. The quality of life in acne: a comparison with general medical conditions using generic questionnaires. Br J Dermatol. 1999;140:672-676.
- Lasek RJ, Chren MM. Acne vulgaris and the quality of life of adult dermatology patients. Arch Dermatol. 1998;134:454-458.
- Campos P.,M.,B.,G., Melo, M.,O.,Mercurio, D.,G. Use of Advanced Imaging Techniques for the Characterization of Oily Skin. 2019 Mar 26;10:254. doi: 10.3389/fphys.2019.00254. eCollection 2019.
- Yoon JY, Kwon HH, Min SU, et al. Epigallocatechin-3-gallate improves acne in humans by modulating intracellular molecular targets and inhibiting P. acnes. J Invest Dermatol. 2013;133:429-440.
- M. Jackson Edward, F. M. T. Robillard Norman The controlled use test in a cosmetic product safety substantiation program.September 2008Cutaneous and Ocular Toxicology 1(2):117-132OI: 10.3109/15569528209051517
- Catambay N., Villanueva J., Verallo-Rowell VM. Comedogencity of virgin coconut (VCO) and other cosmetic oils using a modified Draelos protocol: a randomized double blind controlled trial. Poster presentation at the American Contact Dermatitis Society, 2016 Annual Meeting.
- Verallo-Rowell, V.M., Katalbas, S.S. & Pangasinan, J.P. Natural (Mineral, Vegetable, Coconut, Essential) Oils and Contact Dermatitis. Curr Allergy Asthma Rep 16, 51 (2016). https://doi.org/10.1007/s11882-016-0630-9



[…] flagged as “comedogens” online aren’t because many websites use results of old, outdated, inaccurate Rabbit Ear Assays as their reference. Plus, “comedogens” only clog the hair follicle to cause comedones. […]
[…] flagged as “comedogens” online aren’t because many websites use results of old, outdated, inaccurate Rabbit Ear Assays as their reference. Plus, “comedogens” only clog the hair follicle to cause comedones. […]